Sadness or Depression? Understanding the Difference and When to Seek Support
Sadness is a universal human emotion. It touches all of us at various points in our lives, often as a natural response to loss, disappointment, or transition. Depression, on the other hand, is a mental health condition that extends beyond the realm of typical emotional experience. Yet, it’s not always easy to tell where one ends and the other begins. In a world where emotional language is increasingly used with openness, many people are left wondering: Am I just sad, or am I depressed?
This article aims to offer clarity on the difference between sadness and depression, explore how they show up in the body and mind, and provide guidance on when it’s time to seek professional support. Whether you’re trying to understand your own emotional state or support someone close to you, this is a compassionate space to explore these vital distinctions.
What Is Sadness?
Sadness is a normal, healthy emotional response to life’s challenges. It can emerge after a breakup, the death of a loved one, a personal failure, or even from empathy when witnessing someone else’s suffering. While it can be painful and sometimes all-consuming, sadness tends to be transient and is often tied to a specific event or situation.
Crucially, sadness is not a sign of mental illness. It is one of the many emotions that form the rich tapestry of human experience. According to the American Psychological Association (2023), sadness becomes problematic only when it begins to interfere with a person’s ability to function or persists beyond what might be expected given the circumstances.
When someone is sad, they may cry more easily, feel withdrawn, or lose interest temporarily in activities they usually enjoy. However, they’re still likely to find moments of joy or laughter—whether in the comfort of a friend, a favourite film, or the warmth of a sunny day. Sadness is often accompanied by a sense of emotional resilience, even when things are difficult.
What Is Depression?
Depression, clinically referred to as Major Depressive Disorder (MDD), is a diagnosable mental health condition that affects the way a person feels, thinks, and behaves. It is characterised not only by a pervasive low mood but also by significant changes in energy, concentration, motivation, and even physical health (World Health Organization [WHO], 2021).
Unlike sadness, depression is not always linked to an external cause. Sometimes it emerges without any clear reason, leaving individuals confused and overwhelmed. Depression affects relationships, work, physical wellbeing, and one’s sense of self.
Some of the most common symptoms of depression include:
Persistent low mood or irritability most of the day, nearly every day
Loss of interest or pleasure in activities once enjoyed (anhedonia)
Changes in appetite or weight (either increase or decrease)
Difficulty sleeping or oversleeping
Fatigue or loss of energy
Feelings of worthlessness, hopelessness, or excessive guilt
Difficulty concentrating or making decisions
Thoughts of death or suicide (NICE, 2022)
To meet the criteria for a clinical diagnosis, symptoms need to persist for at least two weeks and represent a change from previous functioning (American Psychiatric Association [APA], 2022).
Sadness is a normal, healthy emotional response to life’s challenges.
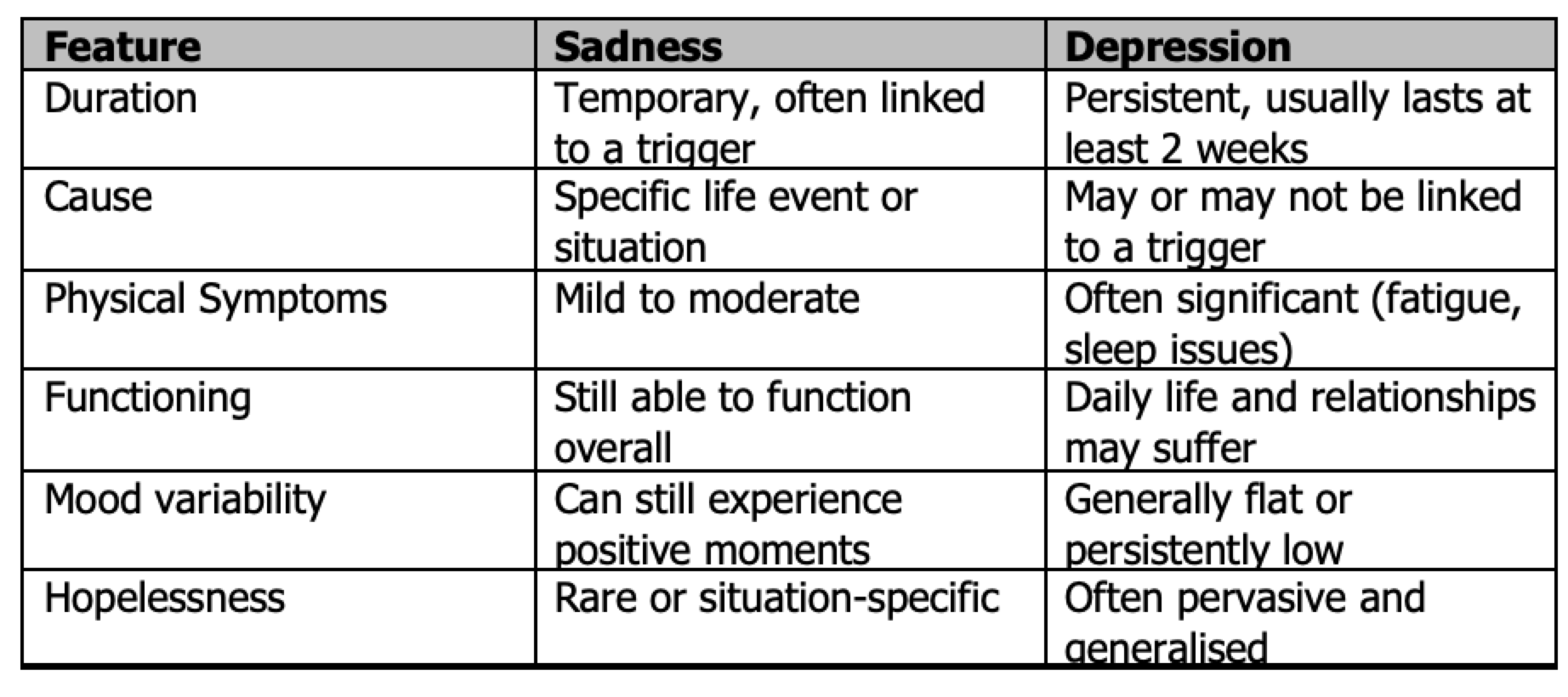
Overlapping Symptoms and Key Differences
While both sadness and depression can involve low mood, emotional pain, and withdrawal, they differ in duration, intensity, and impact.
It’s important to note that people experiencing grief—a natural response to bereavement—may display symptoms like depression, including deep sadness and withdrawal. However, grief typically comes in waves, and positive memories of the deceased remain accessible. Depression tends to feel more pervasive and internally directed (Shear, 2015).
When Sadness Becomes Depression
Sometimes sadness can deepen into depression, especially if the initial emotional pain is prolonged, unsupported, or compounded by additional stressors. For instance, someone who loses their job may initially feel disappointed and sad, but if unemployment continues and leads to feelings of worthlessness, social withdrawal, and lack of purpose, they may develop clinical depression.
Certain risk factors increase the likelihood of this progression:
A personal or family history of depression or other mental health conditions
Long-term or chronic stress (e.g. financial hardship, caregiving responsibilities)
Traumatic experiences (childhood abuse, accidents, loss)
Substance misuse
Lack of social support (NIMH, 2023)
Recognising the shift from sadness into depression is crucial for timely support and intervention. Left unaddressed, depression can lead to worsening mental and physical health, and in some cases, suicidal thoughts or behaviours.
The Importance of Seeking Support
It’s normal to want to manage things on your own. Many people feel that asking for help is a sign of weakness or fear being judged. But depression is not something one can simply “snap out of.” It’s a real, treatable condition—just like any physical illness—and seeking support is a powerful act of self-respect and care.
You should consider reaching out to a mental health professional if:
Your low mood has lasted more than two weeks
You’re no longer enjoying activities that used to bring joy
You’re struggling to sleep, eat, or focus
You feel overwhelmed by hopelessness or worthlessness
You’re withdrawing from relationships or responsibilities
You’re experiencing thoughts of self-harm or suicide
Even if you’re not sure whether what you’re experiencing is depression, talking to a professional can help you make sense of your feelings and develop a plan for support. Early intervention can prevent symptoms from worsening and promote more rapid recovery (Cuijpers et al., 2020).
Recognising the shift from sadness into depression is crucial for timely support and intervention.
Therapies and Support Options
If you or someone you care about is experiencing depression, a wide range of evidence-based interventions are available.
Psychotherapy: Talking therapies can help individuals identify and challenge unhelpful thought patterns and behaviours (NICE, 2022). Integrative psychotherapy, which blends approaches to suit the person, is also increasingly used and valued for its holistic and client-centred approach.
Medication: Antidepressants may be helpful for moderate to severe depression, particularly when used alongside therapy. They work by altering brain chemistry to support mood regulation.
Lifestyle Interventions: Sleep hygiene, regular exercise, social connection, and balanced nutrition can have a significant impact on mood and overall mental health.
Support Groups: Peer-led support groups or group therapy sessions offer a space to feel less alone and hear from others going through similar experiences.
Crisis Support: If someone is experiencing suicidal thoughts, immediate support is essential. In the UK, organisations such as Samaritans (116 123) offer 24/7 free, confidential support.
Sadness Needs Support Too
It’s also important to say that even if what you’re experiencing is “just” sadness, you still deserve support. You don’t need a clinical diagnosis to seek therapy or talk about your feelings. In fact, speaking to a professional while you’re going through a difficult life event can reduce the chances of developing depression and build resilience for the future.
Therapy can offer a compassionate space to process grief, heartbreak, or existential pain—helping you move through sadness with insight, rather than isolation. Emotional literacy and self-awareness are strengths, and seeking support for your mental wellbeing should be seen as a sign of courage, not weakness.
How to Support a Loved One
If someone close to you seems to be struggling, your care and presence can make a meaningful difference. Here are a few ways to support them:
Listen without trying to fix: Sometimes just being there is more valuable than offering solutions.
Avoid minimising: Statements like “cheer up” or “others have it worse” may be intended kindly but can feel invalidating.
Encourage professional support: Gently suggest that speaking to a therapist or GP could be helpful.
Check in regularly: Isolation can worsen symptoms. Consistent, low-pressure contact can be deeply reassuring.
Take care of yourself too: Supporting someone with depression can be emotionally taxing. Prioritise your own wellbeing and seek support if you need it.
A Final Word
We all feel down from time to time. Sadness, loss, and emotional pain are part of being human. But if your low mood has begun to feel relentless, or you can no longer find joy or meaning in the things you love, it might be time to pause and ask: is this more than sadness?
Knowing the difference can be life changing. Depression is common, treatable, and nothing to be ashamed of. With the right support—be it through therapy, medication, lifestyle changes, or simply being heard—healing is possible.
Whether you’re navigating your own emotional terrain or holding space for someone else, compassion is key. You don’t have to walk this path alone.
References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.; DSM-5-TR®). American Psychiatric Publishing.
American Psychological Association. (2023). Sadness. In APA Dictionary of Psychology. https://dictionary.apa.org/sadness
Cuijpers, P., Karyotaki, E., Weitz, E., Andersson, G., Hollon, S. D., van Straten, A., & Ebert, D. D. (2020). The effects of psychotherapies for major depression in adults on remission, recovery and improvement: A meta-analysis. Journal of Affective Disorders, 277, 511–517.
National Institute for Health and Care Excellence (NICE). (2022). Depression in adults: treatment and management (NG222). https://www.nice.org.uk/guidance/ng222
National Institute of Mental Health (NIMH). (2023). Depression: Overview. https://www.nimh.nih.gov/health/topics/depression
Shear, M. K. (2015). Complicated grief. New England Journal of Medicine, 372(2), 153–160. https://doi.org/10.1056/NEJMcp1315618
World Health Organization (WHO). (2021). Depression. https://www.who.int/news-room/fact-sheets/detail/depression